About 8,000 new cases of testicular cancer occur each year in the United States. Although it is rare, it is the most common solid cancer in young men.
The vast majority of testicular cancers arise from germ cells, the cells that normally give rise to sperm cells. These germ cell tumors are broadly divided into two groups: seminomas, which are the most common type, and non-seminomas. In the non-seminoma category, the most common type is embryonal carcinoma. Other types include teratoma, yolk sac and choriocarcinomas. It is common to have different types of cells composing a tumor; these are called mixed germ cell tumors. This is important because the additional treatment plan is based on the type of cancer cells that the pathologist sees under the microscope.
Common questions about Testicular Cancer
The highest incidence is in young men ages 15 to 40. Older men and younger boys can get it, too.
Any boy or man who has had an undescended testicle faces an increased risk of testicular cancer. White men in higher socioeconomic groups have a higher incidence, as well. The reason for this is not well understood.
Testicular cancer usually begins as a painless swelling in the testicle. The earliest detection is probably by self-examination. Occasionally, the testicle is painful. In advanced cases of testicular cancer, other symptoms – such as a cough, abdominal pain or weight loss – may be present.
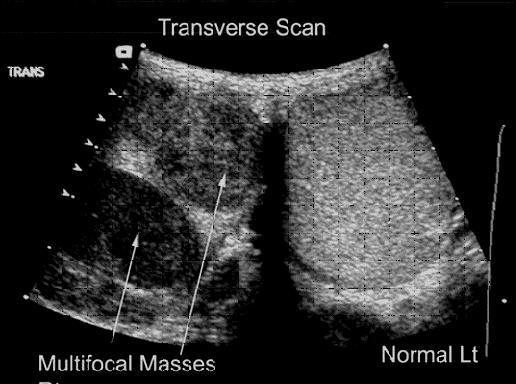
Initially, an ultrasound (diagnostic test producing a two-dimensional image) of the testicles is performed. In addition, a blood test is drawn to check tumor markers. The two most common markers are alpha fetoprotein (AFP) and beta HCG. Most patients also get a chest X-ray and a CT scan to stage the cancer or detect whether it has spread.
Surgery is performed to remove the cancerous testicle. The surgery usually takes about an hour and requires anesthesia. The incision is made in the groin and is typically two to four inches long. The patient can go home the same day, but sometimes will stay in the hospital overnight. Pain can be controlled with oral pain medication. The surgery serves two purposes. First, the surgery removes the primary tumor. Second, the type of cancer is identified. This will give prognostic information and help determine options for additional treatment. Additional treatment is necessary in most cases.
Stage and Tumor Type
The stage of the tumor indicates how far advanced it has become, or whether it has metastasized or spread beyond the testicle.
- Stage I: Contained in the testicle
- Stage II: Lymph node spread
- Stage III: Spread to lungs or other organs
The patterns of spread of testicular cancers are generally very predictable and have been well established. Most commonly, tumor spread is by the lymphatic system. The primary landing site for lymph node metastases, or cancer spread, is to lymph nodes in the retroperitoneum. This region is up near the kidneys.
A CT scan of the abdomen and pelvis is obtained to identify enlarged lymph nodes in the retroperitoneum. If there are enlarged lymph nodes on the CT scan, this indicates at least Stage II disease. Also, a chest X-ray is obtained to identify any evidence that the cancer has spread to the lungs. Cases in which there are enlarged lymph nodes or lung involvement are known as advanced disease. These cases are best treated with chemotherapy.
In cases with no enlarged lymph nodes seen on the CT scan, there is roughly a 20 to 30 percent chance that there still might be microscopic lymph node metastases.
In cases with an elevation of beta HCG or AFP, these markers may give some prognostic information. When the marker or markers are very high, more advanced disease is suspected. If these markers remain elevated after removal of the testicle, this is indicative of advanced disease. If the tumor markers normalize, the cancer is likely to have been contained in the testicle only.
Seminomas never have an elevation of AFP and have an elevation in beta HCG in only 10 percent of cases. In the non-seminoma group, both AFP and beta HCG can be elevated.
Learn more about Siteman Cancer Center’s treatment of testicular cancer.